How to Use Clinical Data in Medical Device Submissions in the EU & US
.png?width=800&height=400&name=How%20to%20Use%20Clinical%20Data%20in%20Medical%20Device%20Submissions%20in%20the%20EU%20%26%20US%20(new).png)
Bringing medical devices to market is still harder than it should be. Obtaining regulatory approval for medical devices is a rigorous process that involves submitting extensive clinical data to governing bodies.
Unfortunately, the risk of product disapproval is very real, and too many manufacturers are forced to extend or repeat clinical studies, resulting in frustration, prolonged time-to-market, and missed revenue targets.
We recently hosted a webinar with our friends at Avania on this very topic, so let’s take a look at the key takeaways and considerations as recommended in “How to Use Clinical Data in Medical Device Submissions in the EU and US.“
Prioritize your clinical data for medical device submissions
In both the European Union and the United States, clinical data plays a vital role in the submission process for medical devices. However, it’s certainly not a one-size-fits-all process.
The regulatory requirements for clinical data are complex and vary by product and market. And while there are methods for efficiently combining clinical data strategies, it’s vital that you first consider each geographic region individually. So, before we get too far into it’s a good idea to establish some baseline best practices.
According to Mary Kay Sobcinski, Sr. Director Strategic Consulting at Avania, there are three solid principles that should guide all clinical studies—in all geographies.
1. Your number one priority is to define your regulatory, marketing, and reimbursement goals in each geography.
Each region has unique regulations, patient populations, and reimbursement programs, and understanding each one individually—as well as how they interact—is crucial work. “I like to think about strategy development and the clinical development plan as your map,” said Sobcinski. “You’ve got to really look at how you’re going to get to your final destination.”
2. Regulatory approval is the first step, not the only step.
When you’re up to your neck in regulatory submission work, it’s easy for teams to put on blinders. But successfully launching a medical device doesn’t simply end with compliance. “You’ve also got to figure out your marketing claims and how you’re going to get someone to pay for it,” said Sobcinski.
3. Clinical and regulatory development is a multi-team (and multi-step) process.
Successfully launching a medical device that spans multiple geographies typically involves multiple teams, such as research and development, regulatory affairs, and clinical research organizations (CROs). Each of these teams plays a crucial role, so a collaborative approach is essential.
It’s not just enough to say you have the best new stent,” said Sobcinski. “You have to be able to demonstrate that to the end users. End users and buyers need clinical data for the decision of switching from one device that’s already on the market, to another one that’s still in process of being approved.”
Optimize your clinical study design for medical device submissions
The best clinical data collection doesn’t happen by accident—it’s a product of intentional design. You should be optimizing your study’s design to get the most out of your clinical data in a medical device submission.
“You have endpoints for regulatory approval, marketing claims, and reimbursement coverage,” said Sobcinski. “And as you are designing your study, you need to be thinking about what those endpoints are and how you’ll be able to collect the necessary data to drive towards those goals.”
The first step in optimizing your clinical data design is to understand the regulatory requirements for medical device submissions in the US and EU, as well as the various legislations you need to cover in each geography.
In the US, the FDA has established a framework for medical device approval that requires clinical data to support safety and effectiveness claims. This means you will need to comply with US federal regulations like 21 CFR 820 and 21 CFR Part 11.
Similarly, the EU’s Medical Device Regulation (MDR) requires clinical data to be collected and analyzed in order to demonstrate conformity with essential requirements. For regulatory submissions under EU MDR, this means adhering to ISO 14155 and GDPR.
BONUS EBOOK: Click here to download The Ultimate Guide to Device Class Requirements Under EU MDR
There are also special considerations for how you design your study protocol. This will include the specifics of your study design, such as the type of study (e.g., randomized controlled trial, observational study), the number of study sites, the duration of the study, and the data collection methods.
It’s important to design a study protocol that is both rigorous and feasible. Your study protocol should be designed to minimize bias and confounding variables, while also taking into account practical considerations such as study site availability and patient recruitment. Additionally, you should be thinking about data poolability across multiple geographies. This means carefully considering your inclusion and exclusion criteria, as well as your sample size.
Combining Clinical Strategies in Multiple Geographies
If you’ve defined your data objectives and optimized the study design for each geographic region, it’s time to start looking for ways to efficiently combine your clinical strategies. Kim van Noort, Senior Medical Writer at Avania, says that the best place to start is at the beginning—with device classification.
“One important factor to consider is whether the device has similar classifications in different regions,” she said. “When there are overlaps, you can really take advantage of those similarities in your clinical study design. However, if there are differences in indications, intended purposes, and clinical benefits, these differences must be carefully considered in the study design and regulatory submissions.”
Another factor to consider is the difference between claiming equivalence versus substantial equivalence. This can have huge implications, especially when comparing the requirements for the EU's Medical Device Regulation (MDR) versus those of the US Food and Drug Administration (FDA). In some cases, companies may need to conduct additional studies to meet the requirements of both regulatory bodies.
Companies should also explore whether there is any existing data in the region that can be used. You may be able to extend your post-market study in one region to a pre-market study in another that includes a new patient population. This can be an efficient way to gather data while also reducing costs.
However, it is important to note that data processing consent (GDPR) must be collected from EU citizens and cannot be integrated into the informed consent form. Furthermore, subject data collected on EU citizens cannot be transferred to the US without consent. While there is no US law that prohibits data transfer to the EU, the California Consumer Privacy Act (CCPA) might require data consent.
Finally, it is important to keep in mind that good clinical practice (GCP) is required in the EU. This means that clinical trials must be conducted in accordance with internationally recognized ethical and scientific standards.
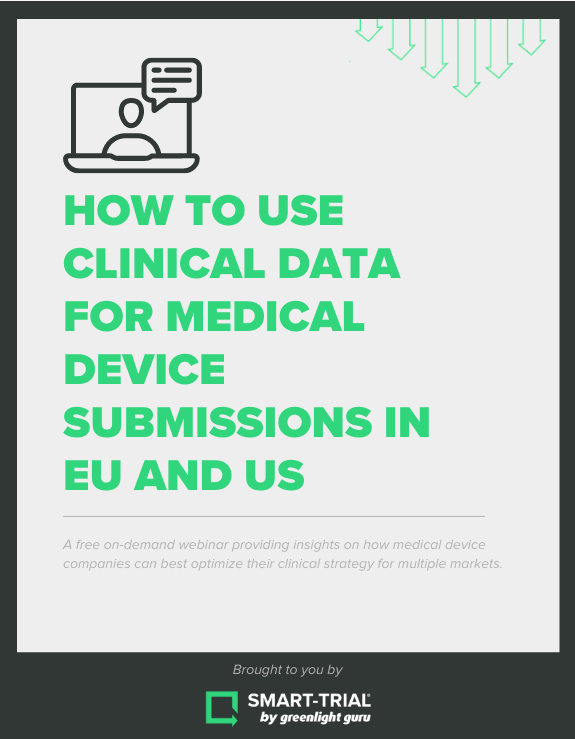
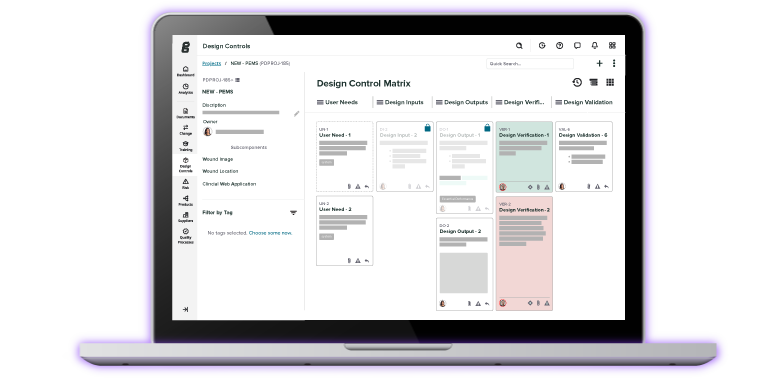
Choose an EDC system that has you covered globally with Greenlight Guru Clinical
If you’re ready to start thinking globally about your medical device submissions, you need a clinical data collection partner who does the same.
Greenlight Guru Clinical is the leading clinical data collection toolbox, purposefully built for MedTech across multiple geographies. Collect and manage clinical data in pre and post-market clinical studies, including registries, cohorts, surveys, human factor testing, design validation, and more.
And take peace of mind knowing that Greenlight Guru Clinical meets the regulatory requirements of the FDA, EU, and most other countries, and ensures compliance out-of-the-box with GCP and ISO 14155:2020.
Ready to get started? Click here to get your free demo of Greenlight Guru Clinical today!
Jón Ingi Bergsteinsson, M.Sc. in Biomedical Engineering, is the co-founder of Greenlight Guru Clinical (formerly SMART-TRIAL). He was also the technical founder of Greenlight Guru Clinical where he paved the way for the platform’s quality standards, data security, and compliance.
Read More Posts
Clinical Trials in 2025: The Outlook for Medical Device Companies
What’s New in Greenlight Guru Clinical 2025.1: Smarter Show Rules and Easier File Vault Access
The Biggest Quality Challenges for Medical Device Companies in 2025
Access the free on-demand webinar
How to Use Clinical Data for Medical Device Submissions in EU and US