IQ, OQ, PQ: A Quick Guide to Process Validation (Plus Free Resources)

What is IQ, OQ, PQ?
These are the abbreviations we use in the medical device industry for the three steps of process validation: Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ). IQ/OQ/PQ ensures that any equipment you use to manufacture your medical device works the way it should—every single time.
In the medical device industry, even one failure in a manufacturing process can lead to devastating consequences for patients, so let’s dig into IQ, OQ, and PQ and the role each of them plays in validating your company’s manufacturing processes.
What does IQ, OQ, PQ mean & how does process validation occur?
-
Installation Qualification (IQ) - Installation qualification is used to ensure that the installation of any necessary equipment, piping, services, or instrumentation has been executed in accordance with the manufacturer's requirements.
-
Operational Qualification (OQ) - During operational qualification, the equipment should be tested to determine process control limits, potential failure modes, action levels, and worst case scenarios.
-
Performance Qualification (PQ) - In the performance qualification phase, the goal is to demonstrate that the process will consistently produce acceptable results under normal operating conditions.
In its guidance on process validation, FDA states that process validation is “the collection and evaluation of data, from the process design stage through commercial production, which establishes scientific evidence that a process is capable of consistently delivering quality product.”
To properly complete process validation, manufacturers must carry out and document all three stages of IQ, OQ, and PQ on the equipment they will use to manufacture their devices. The three stages all validate different aspects of the equipment and its associated processes.
It’s important to note that the phases of process validation must occur in this order: IQ, OQ, PQ. Logically, operational qualification cannot happen until the equipment has been installed correctly; nor can performance qualification happen until the equipment is operating.
What is installation qualification (IQ)?
Installation qualification (IQ) answers the question: “Is everything installed correctly?”
Before you can test whether your equipment performs correctly, you need to know that it has been delivered, installed, and configured correctly. Installation qualification is the documented process that verifies equipment and any parts that comes with it against a checklist of specifications from the manufacturer.
The following steps are often included in IQ:
-
Cross-checking the contents of a package against the packing list
-
Checking for damage to the device
-
Making sure each piece of equipment is installed in the proper location
-
Checking connections to other devices or equipment
-
Verifying the installation of any ancillary equipment
-
Verifying power supply to the device
-
Verifying that the operating conditions and environment match the manufacturer’s specifications
-
Recording calibration and the dates of validation for the equipment used in the IQ
-
Organizing the manuals, certificates, and any other necessary documentation.
What is operational qualification (OQ)?
Operational qualification (OQ) answers the questions: “Is everything operating correctly?” and, “What are the operating limits of this device?”
Once the IQ has been conducted, the next stage in process validation—operational qualification—ensures that the equipment is operating in accordance with the user’s requirements and within the operating range specified by the device manufacturer. In other words, OQ makes sure that the medical device is functioning the way it was designed to.
Operational qualification involves testing all the different functions of the equipment and establishing the operational parameters of the device, which may include:
-
Displays and operational signals, such as LEDs
-
Temperature fluctuation controls
-
Humidity measurement and control systems
-
Fan or motor RPM
-
Servo motors and air-flap controllers
-
Card access and reader
-
Timers and activity triggers
What is performance qualification (PQ)?
Performance qualification (PQ) answers the questions: “Does this process produce the right result?” and, “Is this process safe and consistent?”
While similar to operational qualification, performance qualification is used to verify that the equipment consistently produces the correct results under real-world conditions. That means PQ should be conducted in the actual facility with trained personnel, using the utilities, equipment, control procedures and manufacturing process that will be used to produce commercial batches of the product.
FDA recommends creating a written PQ protocol that includes the following items:
-
The manufacturing conditions, operational parameters, and raw materials used.
-
The data you will collect and the plan for evaluating it
-
The tests you will conduct on the equipment and the acceptance criteria for each
-
An extensive sampling plan that provides confidence of the quality within batches and between batches
-
The criteria for making science- and risk-based decisions about the efficacy of the process
-
The design of the facilities and personnel qualification and training
-
The validation status of the analytical methods used to measure the process, materials, and eventual product
-
The review and approval of the protocol by all relevant departments and the quality team
Once the protocol has been reviewed and approved, then PQ may begin. Afterward, the manufacturer should prepare a report assessing adherence to the protocol, summarizing the collected data, and addressing any manufacturing nonconformances.
When do you use IQ, OQ and PQ?
In 21 CFR 820, FDA also states that IQ, OQ, PQ should occur “where the results of a process cannot be fully verified by subsequent inspection and test.”
In practice, this often includes processes like:
-
Welding, soldering, painting, or heat treating
-
Sterile package sealing
-
Injection molding
-
Aseptic filling
In the case of sterile packaging, for example, verifying the result would require opening it—thereby destroying the packaging and rendering the sterilization process moot.
So, instead of verifying the result, process validation sets out to answer a series of questions that will establish with a high degree of certainty that your process consistently works as it should.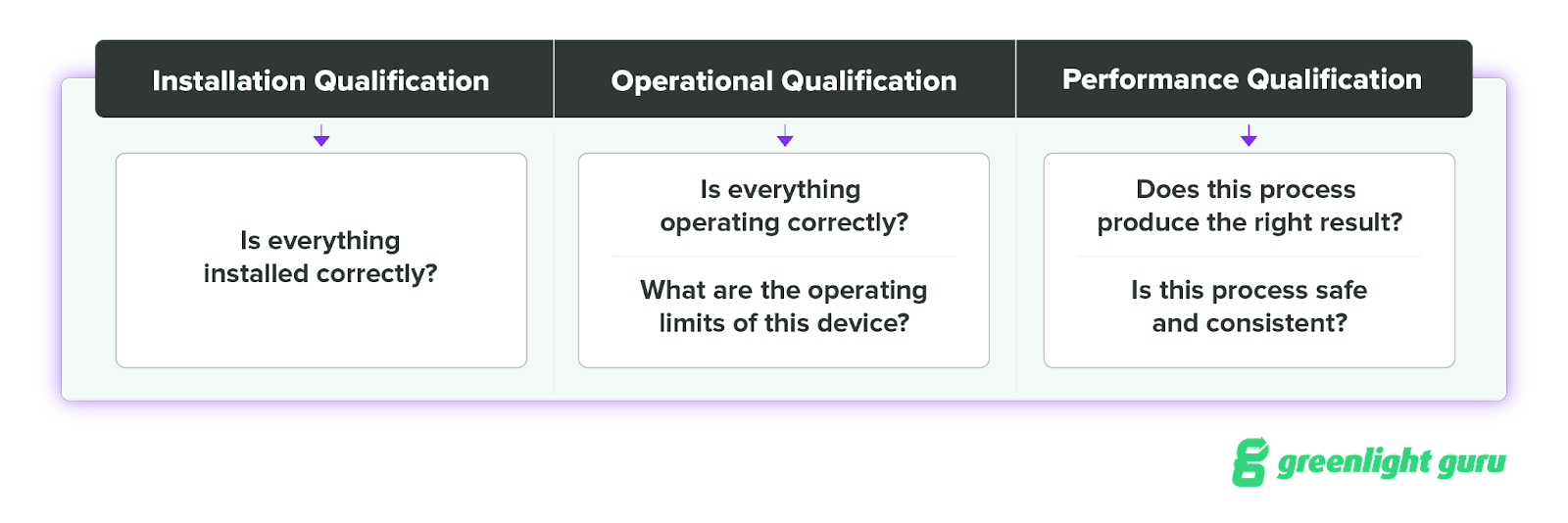
Greenlight Guru's modern approach to software validation gets you up and running faster
In the past, MedTech companies needed to use IQ, OQ, and PQ to validate software as well as manufacturing processes like the ones we just discussed. But today, software validation is done using a modern, risk-based approach known as computer software assurance (CSA).
At Greenlight Guru, we've adopted an automated, risk-based approach to software validation that's aligned with FDA guidance and best practices of standards like ISO/TR 80002-2:2017 and ISO 13485:2016. Our approach to validation keeps you compliant with regulatory standards and ensures you can implement Greenlight Guru quickly and effectively.
If you’re ready to stop worrying about the validation process and do the work you love, then get your free demo of Greenlight Guru today!
Jesseca Lyons is a Senior Medical Device Guru at Greenlight Guru and a Mechanical Engineer by trade who loves working with cross functional teams, including both engineering and non-engineering disciplines. She’s spent most of her career gathering and defining requirements for new product design and development in the...
Related Posts
Explaining the Role of PRRC under MDR & IVDR: Your Questions Answered
Explaining MDCG 2019-11: Software Qualification & Classification for MDR & IVDR
CSV vs. CSA: Breaking Down the FDA's Guidance on Computer Software Assurance
Get your free PDF
Master Validation Plan (MVP) Form