What you need to know About FDA’s Progressive Programs
.png?width=4800&name=podcast_standard%20(2).png)
Are you familiar with FDA’s progressive programs for medical device companies?
Do you know about Expanded Access, the Expedited Access Pathway (EAP) Program, or Breakthrough Devices Program (BDP)? Jon Speer discusses these programs with Mike Drues of Vascular Sciences.
The FDA has created such programs to encourage companies to develop products that meet unmet clinical needs, and reduce the time and cost of bringing new or high-risk products from development to market without actually changing the approval standards.
These programs are not shortcuts and do not involve less work; it’s about businesses implementing a more efficient process.
LISTEN NOW:
Like this episode? Subscribe today on iTunes or Spotify.
Some highlights of this episode include:
- Requirement 1: Allows any device from all pathway categories, if it provides a more effective treatment/diagnosis of a life-threatening or irreversibly debilitating disease/condition.
- Requirement 2: Device must represent breakthrough technology, no approved/cleared alternative exists, offers clinical meaningful advantage over existing/approved alternatives, or availability is in best interest of patients.
- One advantage of BDP program is that it encourages people to come to the FDA very early during the development process; basically just need proof of concept.
- A question never asked in the pre-submission is, “Have we confirmed that we qualify for the BDP.” Questions that were asked were technical in nature.
- 2-Step Process: Take pre-submission to FDA for a BDP designation, and then submit second pre-submission that covers additional items.
- Expedite access of device to market by shifting clinical data requirements from pre-market to post-market.
- FDA is trying to be more progressive and innovative in giving clear and more expedited options of pathways to get medical products to market sooner.
- Average regulatory professionals know the rules, the best regulatory professionals know the exceptions.
Links:
Memorable quotes from this episode:
“(FDA) has had a variety of programs to try to encourage companies on the device side...but also on the drug side...to develop products to meet unmet clinical needs.” - Mike Drues
“The overall goal...was to reduce the time and the cost of bringing one of these new or high-risk kind of products from development to market without actually changing the approval standards.” - Mike Drues
“There’s no shortcuts. There’s still the need to do the work that’s involved.” - Jon Speer
“Regulation is all about the interpretation of words and our ability to defend our interpretation.” - Mike Drues
Transcription:
Announcer: Welcome to the Global Medical Device Podcast where today's brightest minds in the medical device industry go to get their most useful and actionable insider knowledge direct from some of the world's leading medical device experts and companies.
Jon: Are you up to speed with some of the most progressive programs that are available to medical device companies with the FDA, things like the Expedited Access Pathway or the Breakthrough Devices Program? I would encourage you to listen to this episode of the Global Medical Device Podcast to learn a little bit more about these programs as I explore them with Mike Drues from Vascular Sciences.
Hello and welcome to the Global Medical Device Podcast. This is your host, founder and VP of Quality and Regulatory at Greenlight Guru, Jon Speer and sometimes I come across things that they're new and surprising and innovative and exciting to me and they're really progressive types of programs and then I talk to my good friend, Mike Drues, from Vascular Sciences and he's like, "Oh, Jon, this is stuff I've been working on for a long time.", and today's one of those topics where that might be the case and the topic I want to talk about is a couple of exciting new programs from FDA.
One is known as the Breakthrough Devices Program or BDP and the other is the Expedited Access Pathway or EAP so Mike, welcome to the Global Medical Device Podcast.
Mike Drues: Well, thanks Jon. It's always a pleasure to speak with you and your audience.
Jon: You got it and you had sent me an email recently saying, "Hey, these are some exciting programs and programs where you've been doing a lot of work and I confess, I don't know that much about them so do you mind taking a few moments and talking a little bit about BDP and the EAP?
Mike Drues: Yeah, absolutely Jon. Thanks for the opportunity to delve into this very important topic. So, in a nutshell, FDA for many, many years has had a variety of programs to try to encourage companies on the device side of the universe but also on the drug side of the universe to develop products to meet unmet clinical needs and so on. In the expanded access program or Pathway and the Breakthrough Device Program are sort of the latest in that progression of programs. So, starting out with the expanded access pathway, that was originally created back in 2015. It primarily intended to, as I said, encourage companies to develop devices where there's an unmet clinical need in a life threatening or in an irreversibly debilitating disease. This was typically limited to high risk devices, IEPMA Class III devices as well as new or novel devices where there was no predicate so that would include the De Novo.
It's interesting to note that in the original EAP program, the 510(k) was not included in that particular program as we'll talk about that was added later as part of the 21st Century Cures Act in 2016 but basically the overall goal, as most people can imagine, was to reduce the time and the cost of bringing one of these new or high risk kinds of products from development to market without actually changing the approval standards. This is another thing that a lot of people don't understand and that is it's not that we have to do less work, that is it's not that we have to do less testing, bench [inaudible 00:04:04], animal in some cases, and clinical. It's that we're going through the process in a more efficient manner.
But, unfortunately, that part of the program is often not emphasized and I get calls from a lot of companies now wanting to pursue not just the EAP but now most recently, the BDP, the Breakthrough Device Program because they think that it's a shortcut to getting onto the market. They think that it's less work. It's more efficient but it's not less work. We can get into that further as we go Jon.
Jon: Yeah, Okay. So, the key thing I heard there is it's an alternate pathway but it's not a shortcut pathway and I think that's kind of interesting a lot of medical device companies are still looking for that shortcut and folks, if you've heard Mike and I on the podcast before or whether this might be your first time listening to Mike and I chat, there are no shortcuts. There is still the need to do the work that's involved. This is just a more innovative path to try to get that product to market a little bit more efficiently but it's not a shortcut. So-
Mike Drues: That's exactly right Jon and maybe we should fast forward to today because although the Expanded Access Program stills exists, largely it's been replaced, if you will, by the newer Breakthrough Devices Program, the BDP. That, as I mentioned a moment ago, was created at the end of 2016 as part of the 21st Century Cures Act and that Congress, in its infinite wisdom, took a broader approach because among other things, and we can talk about the criteria of the BDP in a moment Jon, they do allow now 510(k) devices to qualify for the BDP. Whether they should or not, that's sort of a [crosstalk 00:06:12] philosophical question but they do and one other thing I'll mention, just a few months ago back in October of 2017, FDA released a guidance specifically on the Breakthrough Device Program.
If anybody is seriously interested, I suggest taking a look at this guidance although to be honest, the only important part of of the guidance, in my opinion, is just the criteria for the program and that's literally copy and pasted from the 21st Century Cures Act so there's really not a lot in that particular guidance and one other thing I'll mention quickly Jon is you and I have talked about the importance of communication with the agency many times including the pre-submission process or the pre-sub.
There is a specific type of pre-sub now that was created specifically for the BDP so for any companies that are seriously considering taking advantage of this option, I would recommend two things. First of all, they should talk to somebody like you or I who does this kind of thing but also they should take a look at the guidance for the BDP Program and they should definitely take this to the FDA as that type of a pre-sub to make sure that they qualify.
Jon: All right, really good tips. And folks, one of the key things that you should know about Mike Drues and his background with Vascular Sciences, I mean, he's worked a lot with not only medical device companies but also the regulatory agencies and if there's an expert in regulatory strategy, Mike's your guy so even if you're looking for that quick path, whatever that might be for whatever reason, it's good that you reach out to him because Mike knows about all of these different programs and the different vehicles and the pre-sub is certainly one of those programs that you and have talked about quite few times and I suspect we'll talk about quite a few more times. It's such a great program for medical device companies to engage with the FDA early in the process to figure out the most viable path for your new technology.
So, Mike, for those companies that are thinking, this might be new to them, the EAP, the BDP, the 21st Century Cares Act and so on, I mean, aside from looking at the guides, how do I determine whether or not something that I'm working on could even qualify. I mean, beyond the guidance is there some sort of device category or some sort of therapy or technology that's better suited for these programs?
Mike Drues: Well, that's a great place to take this conversation further Jon and let's drill into specifically the criteria, the eligibility requirements, if you will, to get into the EAP or now BDP programs and by the way, thank you very much for those very flattering comments. I [crosstalk 00:09:17] appreciate that.
Jon: Oh sure.
Mike Drues: So there's really only a couple of criteria in order to get into this program and like all regulation Jon, as well as on the quality side as well, it's written very broadly, very vague, very nebulous so it can be interpreted in many different ways. First of all, as I said, Congress has expanded the BDP. Devices are now eligible from all pathway categories. I mentioned the IEPMA and the De Novo earlier but they also now includes the 510(k) and pretty much any device regardless of classification as well as regardless of regulatory pathway could possibly be eligible for the BDP Program if it meets the following criteria.
So, the first criteria is that the device provides a more affective treatment or diagnosis of a life threatening or irreversibly debilitating disease or condition. That's criteria Number 1 and criteria Number 2, you're required to meet at least one of the following criteria. The device represents a breakthrough technology and of course, how we define the phrase "Breakthrough Technology" is largely up to us especially. We know Jon that the vast majority of folks in our audience are working on 510(k) devices, on one hand, it's pretty hard to argue that a device that's eligible for the 510(k) is a breakthrough technology if it's substantially equivalent to another device already on the market. But, it can be done and I've actually had a few devices successfully under the BDP program as a 510(k) so it depends on how you define breakthrough technology.
Another criteria is that no approved or cleared alternative exists. Now again, that seems contrary to the 510(k) but this is right out of the 21st Century Cares Act so you can spin this a little bit, maybe if you're labeling is a little bit different, maybe if you're technology is a little bit different. My favorite example is if you have a device on the market that's currently being used off-label, then technically, no other approved or cleared alternative exists because as you know Jon, FDA doesn't regular the practice of medicine so if a device is being used off-label, then that could qualify here. The third, and by the way, we have to meet one of these four requirements. Not all four of them although I always try to write it. I am writing a BDP justification for a product right now and we're trying to address all four criteria. So, the third criteria is the device offers some clinically meaningful advantage over existing approved or cleared alternatives.
For example, a decrease in hospitalization or an increase in quality of life. I would like to think, Jon, that all devices do that regardless of whether or not they qualify for this program.
Then the fourth is a really touchy feely one; that is the ability of the device ... sorry, the availability of the device is in the best interest of patients. Again, I would like to think that would apply to all medical devices not just BDP devices but that's exactly what the 21st Century Cures Act says.
Jon: Okay.
Mike Drues: Let me just repeat 'cause I went through that pretty quickly. Let me just repeat the first criteria is the device provides more effective treatment or diagnosis of a life-threatening or irreversibly debilitating disease. That's requirement number 1.
Requirement number two, we have to meet at least one of the following: the device represents a breakthrough technology; there's no other approved or cleared alternatives; the device offers clinically meaningful advantages over other existing devices, and finally the availability of the device is in the best interest of the patient.
I can't emphasize this last point enough, Jon. That's exactly what the regulation says. How we interpret that regulation is 100% up to us. As I like to say, regulation is all about the interpretation of words and our ability to defend our interpretation. Those are the words that I just shared with you and your audience right out of the regulation. How we interpret those words is totally up to us and how we go and sell our interpretation to the FDA is totally up to us. I've never bought into the logic that somebody that seemed to think and that is that somehow the FDA's interpretation of a certain set of words is more correct than my interpretation. It's just simply they don't know anything more than we do.
Jon: If I squint, I can almost see just about every medical device known to man could almost fit into those criteria, right?
Mike Drues: Not to be cynical, Jon, but I think you are exactly right. Not to get off on too much of a tangent but quite frankly, we can't underestimate the importance of politics here because when you look at how this regulation, specifically the 21st Cures Act came into play and again, I don't want to get too politically technical here, but when you look at the number of electoral college votes coming from the states with the largest medical device companies, you start to understand why regulation gets written the way that it is.
Congress is casting a very broad net here. As I said earlier, whether they should or not, that's a different topic but that's the regulation, as I said, it's now up to us to interpret it. The result is I'm getting lots of calls, a growing number of calls from companies ... "Hey we've heard about this breakthrough device program. Is this something that we can take advantage of? Is this something that will allow us to get our device onto the market quicker or easier?" Kinda like the wellness exemption. I would put it in the same bucket as we've talked about that before as well.
Jon: Sure. Obviously, mechanics aside, I guess I'm a little curious. Have there been any technologies that you're aware or that you've worked on that you are able to disclose, of course, that have been through this program successfully?
Mike Drues: Let me say it this way. I've taken now probably about five or six devices. Remember specifically the BDP was only created less than a year ago so I've taken about five or six devices to the FDA specifically for the BDP. The vast majority of those have qualified for the BDP program. In other words, FDA says they've bought into our arguments for the justification and we can go into that in more detail, how we do that justification, if you want.
I'm just a little bit reluctant to mention the specific ones, Jon, because those are in the BDP program now. They're still under development. They're still under review.
Jon: Sure, sure.
Mike Drues: By the way, one of the advantages of the BDP program and this is something that I actually agree with FDA on, is they encourage people, or at least they say they encourage people, to come to the FDA very early in the development process. You do not have to have a ... you do not have to be at the point of design freeze. In some cases, you don't even have to have a working prototype. You can to a certain extent go to them with a concept which what I call a virtual device and say, "We're intending to design the device to work this way. We're intending the device is going to do this, this, and this. If assuming that we can do all these things, would it qualify for the BDP?"
That's the essence of the program. If Congress and the FDA really want to encourage companies to bring these kinds of new and novel high risk devices to market as soon as possible, that's the kind of very early collaboration that we need between the company and the FDA.
Jon: You know, I really like that point, last point a great deal. Let me pull in some recent discussion that I saw. I don't remember exactly which group but one of the medical device groups on LinkedIn someone had posed a question about proof of concept. Is there any value in proof of concept in today's day and age? I'm a big fan.
I think there's always value in proof of concept and you've just given a regulatory reason for why proof of concept has a lot of credence because I don't have to have that design freeze. I can have a concept, even a virtual concept in this case, and be able to present that to FDA to determine this alternate pathway to get my device cleared which, you know, knowing that pathway, how I'm going to pursue the regulatory waters, if you will, is important to a lot of things form a product development standpoint.
It determines in large cases all the things that I need to do whether from a pre-clinical or a clinical standpoint. It may even influence how much ... actually let me recant ... it most definitely will influence the amount of funding that I'm going to need during the design and development efforts to commercialize a product. I really like that concept of being able to go to the FDA with an idea really to help determine this pathway.
Mike Drues: I'm glad you do, Jon. I very much like it as well but I gotta be honest with you and your audience. I wouldn't be doing my job if I didn't point out not just the good but the bad and the ugly as well. That is, FDA is not used to that. In spite of what the politicians will have us believe and in spite of what the guidance might say, they're not used to seeing devices very early in the product development cycle. They're much more used to seeing devices either at the point of design freeze or very close to the point of design freeze.
Even though FDA publicly, and this is not a criticism, just an observation, at least based on my real world experience, even though FDA says these things that's not necessarily always what happens in reality. I can share with you, one case, one situation I'm involved in right now. The company went to the FDA trying to qualify for the BDP program (a break through device program) and were unsuccessful. FDA basically said no and then they asked me to come in and help which is unfortunately often the case. If they would have asked me to help first, they probably wouldn't be in this situation but nonetheless, in doing a little forensic analysis, I've realized a couple of things.
First of all, I realized that as part of the pre-sub, one of the questions they never asked was, "Have we confirmed that we qualify for the BDP?" That's number one. Don't overlook the obvious.
Number two, the responses that the questions that FDA did give back were all technical in nature. I mentioned earlier, Jon, the breakthrough devices program guidance that came out the end of last year.
One of the important things in that guidance and I personally disagree with this but this is what it says in the guidance is that a BDP pre-sub should be limited only to the BDP status.
In other words, you cannot combine it with a more traditional pre-sub where you would include regulatory strategies which includes testing matrix, you would include clinical data and so on, and so on. In an ideal world, I would like to do one pre-sub where we include both the BDP designation as well as those other things but at least for right now, according to the guidance. By the way, guidance is guidance. It's not binding but we have to do it in a two step process.
What I advise the companies I work with who are interested in doing this is take this to the FDA first as a first pre-sub specifically focusing on the BDP designation and then follow that up with a second pre-sub, a more traditional pre-sub, where you cover those other things that I mentioned and that you and I have talked about many times before. I think that makes the process more inefficient. That's why I don't like it.
More importantly, I think that the breakthrough designation of breakthough device program needs to be taken into context with all those other things but at least for right now, that's the way the mechanics are working. I would like to see that change but at least for right now, that's the path that I'm taking with the companies I'm working with.
Jon: Okay. The promise of the program is that it would ideally be more expedited or more efficient review with the FDA and I know you may be ... it still a little too early to know. You mentioned you have several that are in with the FDA right now.
Give me your anecdote. Give me your ... has the process been smoother generally speaking? Has it been more predictable? What kind of anecdotes can you share about-
Mike Drues: Well, one other thing-
Jon: -so far?
Mike Drues: One other thing I can mention in terms of making the process more efficient or even quicker for companies. Look this is not a panacea. This is not a magic pill. As I said earlier, the requirements are essentially the same whether you're in one of these programs or not. However, one of the ways that we can speed access of the device to market ... as you know Jon there's always been a healthy competition between the US and the EU in terms of what devices and drugs come onto the market first in which place. Well, one of the ways that we're mitigating that time here in the US is by shifting some of the clinical data requirements from pre-market to post-market. In other words, for class 3 devices that usually require clinical data, and even for class 2 devices under a de novo or a 510(k) that might require clinical data, one of the advantages of getting into one of these programs is that you may be able to shift some or perhaps even all of your clinical data, your clinical burden as I like to call it, from pre-market to post-market and obviously that had advantages for the company.
As I said, I can't give you overall statistics with regard to the BDP program, I'm not even sure that if any of them are publicly available because the program is so new, and I'm not sure as part of MDUFA if FDA is required to collect statistics specifically on these programs. They might, I just don't know. But I can tell you the EAP that's been around for a little longer, when it was created in 2015, there were 29 EAP applications. 17 were accepted, a dozen of them were rejected, and usually those decisions were made within 30 days or less. Another advantage of the EAP, and now the BDP as well, is if you put a package together and submit it to the FDA for this designation, you will probably get a response, a decision from FDA, within a pretty short period of time. Technically, according to the guidance, it's supposed to be 30 days or less, but like all of those statutory numbers, I take them with a big grain of salt. Bottom line, we're not talking about months and months and months, but we should have a decision within a month or maybe a little bit more.
Jon: Right. And I guess part of what I want to ... I guess I'll use the word predict, so to speak, is where's the puck going, so to speak? Where is the FDA, in this case, where are they moving towards? You and I've talked a lot about today on these exciting programs, the EAP and the BDP, but we've talked about other programs in the past. We've talked about the accelerated 510(k), the recent news on that, and some of the other -
Mike Drues: The alternative 510(k).
Jon: The alternative, yeah, I'm sorry ... and some of the recent news on these different regulatory pathways, and if I'm to predict where I think is agency is trying to move towards is being a little bit more progressive. I'll use the word innovative, it may not be the right use of the word in this case, but certainly progressive, and giving clear options, or more expedited options, to industry on pathways to get products to market faster. I think I was at an event recently, a couple months ago, and there was heavy FDA participation in this particular event and actually Dr. Shuren presented. He was presenting the video conference, but one of the things that he said was, and I don't remember the exact numbers but, the FDA has been looking at the time that it takes to get new products to market in the US and it was something like the US was 27th in the world as far as countries to bring new technologies to market, and FDA is very cognizant of that, and FDA's hope and promise is to be number one in the world in bringing new innovative medical technologies to the world and it seems like these types of programs are in that spirit.
Mike Drues: Well, I would agree Jon. I think a lot of these programs are in that spirit, to use your phrase. But I'm not sure being number one in terms of the quickest to market should be our overall goal, because one of the things I learned 25 years ago when I started out as an R&D engineer is you can have something good, or you can have it fast, or you can have it cheap. It's very difficult to have all three of those things at the same time. Should our goal be simply to get products on the market as fast as we possibly can, or should our goal be to get products onto the market as fast as we can that are also safe and effective and do what they do, and so on and so on? So there's a balance here. There's a fine line here. And listen, I'm not gonna say anything specific about individuals at FDA and whatnot, but we cannot de-emphasize the importance of politics here. I alluded to a moment ago what I think is a healthy competition between the US and the EU and other parts of the world as well. The politicians are painfully aware of this. So there is a balance.
Jon: For sure, for sure. Mike, I appreciate your insights and your experience on these newer programs from the FDA. Any other closing thoughts on EAP or BDP or 21st century cures in general that you'd like to share with our audience today?
Mike Drues: Yeah, so just to wrap this up Jon, what I would like to leave the audience is with this: one of my many favorite regulatory mantras are "Average regulatory professionals know the rules. The best regulatory professionals know the exceptions." We are talking here about programs that are less commonly used. But, in certain situations, in certain circumstances, they can be very important, they can be very valuable to both the company as well as to society and patients in general.
So people need to be aware of these programs, at least in a general sense. And if you're seriously considering the use of one of these programs, specifically the BDP, take advantage of the BDP pre-sub option. Take it to the FDA. Provide a very strong justification as to why your particular device meets those criteria that we discussed earlier in today's podcast. I personally like to write this as sort of a call and response. In other words, here's criteria number one, here's why my device fits. Here's criteria number two, here's why my device fits, and so on. As I said, technically you only need to meet one of those four criteria in the second batch. I try to meet as many as I can, even all of them ideally. Remember, for the BDP pre-sub, you need to limit that, at least for right now, to just the BDP designation, which means that you can be fairly light on the device description, on your technology, on your regulatory strategy, on your clinical burden. I guess theoretically, you could leave all of that information completely out. I don't do that, I do try to provide FDA at least some of that information, but perhaps not in as much detail as I would in a traditional pre-sub.
Bottom line, Jon, no matter what pathway to market that I'm using, whether it's BDP or something else, I want to demonstrate to my friends on the FDA side of the table that I know what the heck I'm doing. Yes, I'll listen to their suggestions and so on, but at the end of the day this is my party not theirs, and it's important to remember who ultimately is in control here.
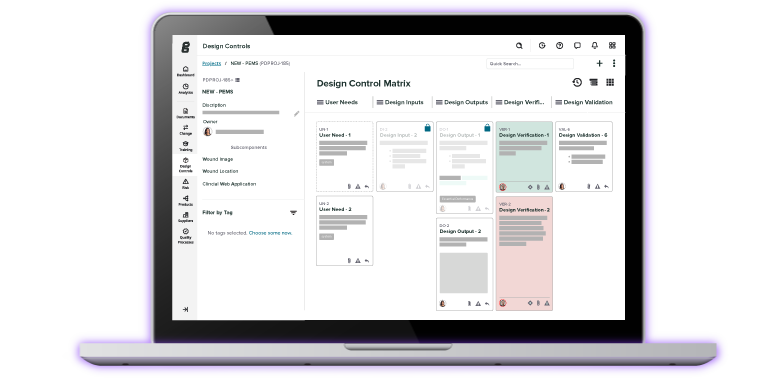
Jon: Great advice. And folks, again I want to stress and re-emphasize the BDP, the EAP, these are not shortcut paths. You still have to do the work. A big part of that work is gonna involve solid design controls and risk management. That's a key aspect of any device that's under development. Making sure you have solid design history files established throughout the entire product realization process is so important. That's one of the things that we do at Green Light Guru is we built an EQMS software platform specifically for the medical device industry, and we have designed specific workflows for managing design control activities and risk management and how that dovetails into your entire QMS is a big part of what we do at Green Light Guru. So if you'd like to learn a little bit more about how our program can help you support your regulatory pathways and these exciting programs from the FDA, as well as the traditional programs of PMAs and 510(k)s, and if you're in Europe, CE Mark technical files, I would encourage you to go to www.greenlight.guru to learn more about some of the things that we're doing.
Mike -
Mike Drues: Jon, before we wrap this up, can I just add one last thing?
Jon: Of course.
Mike Drues: I know we're running short on time, but just one last piece of advice for your audience, cause I see a lot of people make this assumption or even mistake as well. We talked earlier about unmet clinical need. Well, a lot of people will assume that if other devices are on the market that are intended to do the same thing, that there is not an unmet clinical need. In other words, there cannot be any other device on the market that does that. I do not take such a literal interpretation to the phrase "unmet clinical need." Many times I will argue that my device is serving an unmet clinical need, even if there are other devices on the market that do the same thing. If I can argue that ... let's be honest, the other devices out there do a crappy job. And I will ask physicians or surgeons or whoever it is, for example, to write letters as subject matter experts to basically say yes, there are other devices on the market that say they can do this, but they don't do it very well, therefore there is an unmet clinical need for this new device. So I just wanted to throw that particular thing in there-
Jon: That's a good tip.
Mike Drues: ... cause I see a lot of companies do that, and from a regulatory perspective, one of the big advantages if you can be successful in convincing FDA that you're meeting an unmet clinical need, your regulatory burden is reduced even further. So, obviously that's a huge advantage for the company.
Jon: Terrific advice. Folks I wanna thank my guest once again today, Mike Drues. Mike is with Vascular Sciences, you can reach out to him, find him on LinkedIn. If you wanna get in contact with him and you can't find his contact information or his exciting articles and content on various topics in the regulatory realm, just reach out to us and we'll get you connected. But Mike, thank you once again.
Mike Drues: Thank you, Jon. Always a pleasure.
Jon: Alright folks, you've been listening to the Global Medical Device podcast and this is your host and founder and VP of Quality and Regulatory at www.greenlight.guru Jon Speer, and tune in again real soon.
ABOUT THE GLOBAL MEDICAL DEVICE PODCAST:

The Global Medical Device Podcast powered by Greenlight Guru is where today's brightest minds in the medical device industry go to get their most useful and actionable insider knowledge, direct from some of the world's leading medical device experts and companies.
Nick Tippmann is an experienced marketing professional lauded by colleagues, peers, and medical device professionals alike for his strategic contributions to Greenlight Guru from the time of the company’s inception. Previous to Greenlight Guru, he co-founded and led a media and event production company that was later...