Building an Effective CAPA Program: Key Steps and Common Challenges
The process for taking corrective actions and preventive actions (CAPA) is one of the fundamental elements of every MedTech quality management system. Without a well-defined CAPA program, there is a huge risk that you may miss systemic issues in the design, development, and manufacture of your medical devices.
And yet, despite the importance of CAPA, companies often struggle to carry out their CAPA program effectively. This can happen for a number of reasons (which we’ll look at), but it often comes down to problems with how the CAPA process was defined in the first place.
So let’s take a look at the key elements of a good CAPA program—and what to avoid as you go through the CAPA process.
What is a CAPA Program?
Your CAPA program is a standardized process for investigating and addressing systemic issues within your business, like a component that is repeatedly failing inspections during the manufacturing process. Establishing and maintaining procedures for a CAPA program is a regulatory requirement, laid out in 21 CFR Part 820.100, Corrective and Preventive Action. The same process is similarly defined in ISO 13485:2016, in sections 8.5.2 and 8.5.3.
5 key stages of a CAPA program
An effective CAPA program consists of five stages and requires a methodical approach to carrying out the steps in each stage. Each component of your CAPA process builds on what came before it to create a comprehensive program for identifying, investigating, and correcting or preventing systemic issues in the production of your devices.
Here are the five key stages of a compliant CAPA program:
1. Identify potential CAPA quality cases
In order to identify potential CAPA cases, you need to monitor your quality processes for potential issues. These CAPA inputs include:
- Non-conforming material report (NCMR)
- Internal and external audits
- Management reviews
- Validation activities
- Risk analysis
- Clinicals
- Complaints
Once you’ve spotted a potential CAPA case, the next step is to document it with a CAPA request. A CAPA request is simply a description of the possible CAPA, a detailed list of its probable sources, any available evidence, and an explanation of how the information was reported.
From there, a quality review board (QRB)—a group consisting of strong cross-functional representation—should review the request to determine whether a CAPA investigation should take place.
2. Prepare for your CAPA investigation
If the QRB determines that a CAPA investigation is justified, the next step is to make sure you’re fully prepared for the investigation. You can begin by assigning the new investigation a unique ID number for tracking and reference purposes. Then, identify the parties, processes, procedures, and departments that may be associated with the CAPA. Be as thorough as possible here.
Keep in mind that there are six potential sources for a quality problem:
- Method
- Material
- Machine
- Manpower
- Measurement
- Mother Nature (AKA, environment)
Determining the sources, products, and processes involved with the CAPA will help you to identify the people you need on the team overseeing the investigation. For example, you might need engineering, marketing, manufacturing or regulatory as part of your team.
3. Investigate the root cause of the issue
With your data, sources, and team in-place, it’s time to get down to business. The first step here is containment. This might mean stopping production, switching to a new parts supplier, or issuing a recall—whatever is required to prevent the issue from becoming more widespread.
Once the problem is contained, you can turn your attention to the root cause of the issue. 21 CFR 820.100 states that manufacturers must have established procedures for “investigating the cause of non-conformities relating to product, processes and the quality system.” This refers to your root cause analysis (RCA)
There are many different methods for root cause analysis::
- Five Whys is a process of asking successive questions based on the answer to the previous question.
- Fishbone Diagram is a visual way to sort potential causes into categories branching off from the original problem.
- Flowchart is a method of mapping the process through the different pathways in the organization to identify potential sources of the issue.
- Pareto Chart is a graph used to visualize the most likely sources of an issue.
- Scatter Diagram is a comparative way to plot pairs of data points to determine correlation.
What’s most important is that you choose a method and follow it all the way to the end, wherever it leads. Poor RCA is a major source of problems in CAPA programs.
4. Implement and document your CAPA quality action plan
Once the root cause analysis is complete and you know what’s causing the problem, you need to develop what’s typically called a CAPA quality action plan. This is the document that contains the specific steps, SOPs, roles, reporting requirements, and expectations as you implement your corrective and preventive actions.
There are three kinds of problem-solving actions typically used:
- Corrections refer to actions taken to immediately address a problem or non-conformance. They are focused on fixing a current issue and do not necessarily prevent the problem from occurring again in the future.
- Corrective actions, on the other hand, are longer term solutions that are implemented to address the root cause of a problem and prevent it from occurring again.
- Preventive actions, also known as preventive measures, are proactive steps that are taken to prevent problems or non-conformances from occurring in the first place.
In addition to the type of action, CAPA quality action plans should include:
- Due date
- Action description
- Responsible person
- Plan for effectiveness check
- Verification of effectiveness checks (VOE)
5. Verify CAPA effectiveness with management review
The final foundational step of CAPA is perhaps the most important, as it determines whether your CAPA quality program is functioning as it should.
In this step, the CAPA goes back to the cross-functional team and the MRB or Quality Review Board for assessment. They should be checking to see whether:
- The CAPA resolved nonconformances;
- The preventive actions have been effective;
- The CAPA actions have caused any new problems.
Companies sometimes struggle with effectiveness checks, particularly in choosing the right method of verification. Thankfully, there are some tried and true methods for verifying effectiveness of your CAPA quality issue:
- Trend analysis in which you review data over a specific period of time to determine if the problem occurs again.
- Periodic checks in which you schedule time for the quality board to review that a process has been corrected.
- Surprise audits in which you audit with no announcement, to confirm if the procedures and actions are being followed by your team.
- Sampling in which you verify corrective actions by using a subgroup of data as a representation of the whole dataset.
And I’d be remiss if I didn’t remind you that everything you do during the CAPA process must be documented and retained for your records.
Common challenges in CAPA management for medical device companies
While the five phases we’ve discussed may seem fairly simple, in reality, there are many different ways to mishandle or misuse a CAPA program. Some of the most common problems with CAPA include:
Poorly defined CAPA process
Your CAPA program is only as good as the process you have in place to carry it out. So it may surprise you to learn that many companies do not have a well-defined CAPA process in place. In fact, the lack of a defined CAPA process is typically the number one reason FDA issues 483 observations to MedTech companies each year.
The problems with a CAPA process usually come down to three issues:
- You haven’t defined a CAPA process.
- You have defined a CAPA process, but it isn’t compliant with the regulations.
- You have defined a CAPA process and it is compliant, but it isn’t being followed.
If you think you fall into any of those categories, then check out our Ultimate Guide to CAPA, where we take a deep dive into each stage of the CAPA process and explain the exact steps that a compliant, effective CAPA program will have.
Overuse or underuse of CAPAs
A lot of companies end up overusing or underusing their CAPA program to the point that it begins creating more problems than it solves.
Some companies will get “CAPA happy,” opening a CAPA for every nonconformance they find or complaint they receive. And while a nonconformance or complaint might be indicative of a systemic issue, that’s not always the case. When companies overuse their CAPA program, they end up with dozens of open CAPAs that put an enormous strain on the business without really solving anything.
Underuse of a CAPA program, on the other hand, may be an even bigger issue. If systemic issues are going unnoticed and/or unaddressed at MedTech companies, that will lead to issues with the product and can easily lead to harm to patients.
Inadequate root cause analysis
A proper RCA requires a good amount of time, effort, and discipline. It’s not unusual for companies to skimp on the RCA and simply restate the problem and its description—and call that the root cause.
But if you’re not using a proper RCA technique and following it to its conclusion, you probably won’t find the root cause of the issue. And you’ll be doing all of this again when you realize the problem persists.
So, I’d recommend using a proven RCA technique like the ones I mentioned earlier. But be sure you’re following the RCA process to the very end. Otherwise, you’ll be spending an enormous amount of energy almost fixing an issue.
Greenlight Guru simplifies CAPA management
The truth is that even with a well-defined CAPA program in place, carrying out the full CAPA process can be a huge task. Companies that struggle to close out CAPAs often have the right procedures in place, they just have trouble executing.
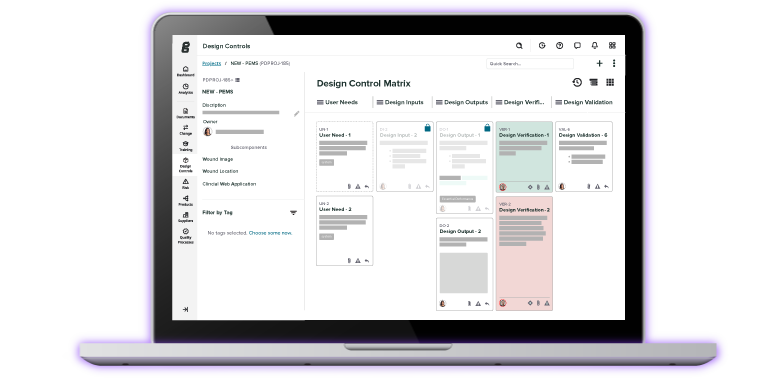
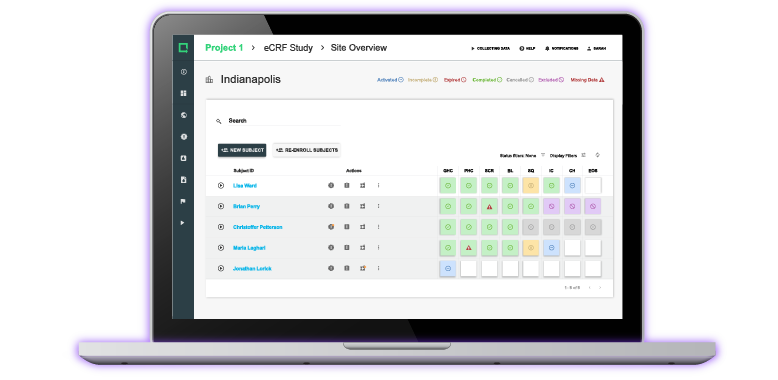
But with Greenlight Guru Quality, you’ll have everything you need to keep your CAPAs moving and ensure that you correct or prevent problems within your business before they have the chance to do real harm.
With Greenlight Guru Quality, you’ll have a dedicated CAPA management workspace that is fully integrated with the rest of your QMS, making it easy to link CAPA inputs to an investigation and ensure you’re always working with a single source of truth. You’ll also be able to create a CAPA team, assign tasks, create custom workflows and automations, and view progress at any time—keeping you on track to close out your CAPAs in a timely manner.
Ready to see how easy CAPA can be with Greenlight Guru? Contact us today for your free personalized demo!
Etienne Nichols is the Head of Industry Insights & Education at Greenlight Guru. As a Mechanical Engineer and Medical Device Guru, he specializes in simplifying complex ideas, teaching system integration, and connecting industry leaders. While hosting the Global Medical Device Podcast, Etienne has led over 200...
Related Posts
5 Foundational Steps of a CAPA Quality Process
Ultimate Guide to Corrective and Preventive Action (CAPA) for Medical Devices
CAPA Best Practices: 4 Tips for Building an Excellent CAPA Process
Get your free PDF
CAPA Report Template